Researchers say retroviruses that are dormant in our genome can be triggered by environmental factors and cause diseases such as multiple sclerosis.
 Share on Pinterest
Share on PinterestThe human genome is a veritable graveyard of dead retroviruses, making up somewhere between 5 percent and 8 percent of our DNA, according to most credible estimates.
These retroviruses make up much of the junk DNA in our bodies — in essence, leftovers from millions of years of evolution that have been deactivated and set aside.
Sort of like the trash folder on your computer before you empty it.
Spooky, perhaps, but previously thought to be harmless. Except many scientists now aren’t so sure.
Recent research suggests that these human endogenous retroviruses, or HERVs, could, under the right conditions, rise zombie-like to wreak havoc on our bodies.
They may even be at the root of conditions such as multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS), and even schizophrenia.
First, let’s talk a little about what a retrovirus is.
In the simplest terms, a retrovirus works by inserting its genome into the DNA of a host cell, thus replacing some of the cell’s “code” with its own.
In humans, the most well-known retrovirus is probably the human immunodeficiency virus (HIV). This is why the common therapy for HIV is antiretroviral drugs.
Most retroviruses are exogenous, which means they attack a person from outside the body and are transmitted through fluid, air, or other contact.
HERVs, by contrast, are endogenous, meaning they’re already within us, coded into our DNA.
These are remainders from when our primordial ancestors were infected with retroviruses. Some of this code got left behind, while their harmful effects were mutated away.
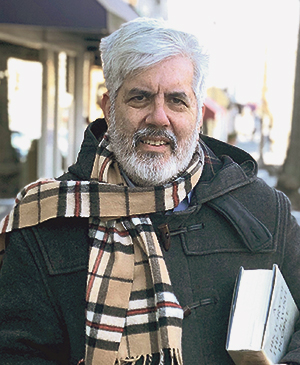
“During evolution, retroviruses were vectors of genetic diversity, jumping from species to species,” Hervé Perron, PhD, one of the pioneers of HERV research and the founder of GeNeuro, a pharmaceutical company developing HERV-specific treatments, told Healthline. “These retroviruses can recombine with the host gene first, so they can embark genes and infect cells while retro-transcribing their genetic information.”
That’s opposed to retroviral cells like in HIV, where only infected cells have inserted copies in their DNA so they are not transmitted hereditarily.
HERVs, by contrast, stick around because these retroviral infections occurred in a significant number of instances in regions that wouldn’t affect the life of the newborn. And so they persisted in our genome.
In some cases, researchers speculate these dead viruses might even have some beneficial effects, including helping form a prototype immune system as viruses fought other viruses for supremacy.
Any benefits aside, HERVs are supposed to stay dead. A live retrovirus is an infectious agent, not a happy companion.
“Many of these HERVs have contributed to physiological function being adopted by the genome, while others remain latent and dormant but retaining pathogenic potential of their viral origin,” Perron explained.
The problem, scientists have been exploring, is when environmental and other factors trigger these HERVs, waking them up from their deep slumber.
“Dormant HERVs can be reactivated by environmental factors such as inflammation, mutations, drugs, or infection with other viruses,” said Dr. Patrick Küry, lead author of a new paper on neural cell responses to HERVs in the journal Frontiers in Genetics.
Furthermore, “Even if they were coming from an endogenous copy, the final product of this expression are proteins that might in some circumstances make virus-like particles,” Perron explained.
These retroviral reactivations might be the missing “environmental” link making the difference between someone developing MS or ALS or remaining healthy, Küry said.
“MS is caused by direct autoimmune attacks on myelin — the fatty coating of nerve cells — in the brain and spinal cord, but we don’t yet understand how these attacks are triggered,” he wrote in a press release. “Subsequently, it was shown that levels of HERV RNA and protein — the ‘readouts’ from reactivated HERV DNA — are increased in the brain and spinal cord fluid of sufferers, as well as in their brain tissue postmortem.”
In essence, the theory is that HERV proteins trigger an immune reaction that damages myelin and can trigger MS, the researchers say.
If this theory bears out — and there are clinical studies, trials, and therapies in the works — then we might be able to develop more effective treatments for these degenerative diseases.
For instance, if HERV protein-neutralizing antibodies work to help treat these conditions, it would demonstrate concretely the role these retroviruses play in these disorders and pave the way for new therapies.
A study published in March by researchers from the University of Basel in Switzerland added weight to this theory.
Those researchers noted a “magnetic resonance imaging sign compatible with the remyelinating potential” of an antibody that attacks the enveloping protein of a HERV in treating progressive MS.
That’s significant since repairing myelin could be key to undoing some of the damage of MS.
Over at GeNeuro, Perron and his team have also been exploring these HERV protein-attacking antibodies.
“Given the load of HERV protein that is expressed in autopsies and brain material that we detected in patients, we realized we should first neutralize this protein, so we’ve bred and selected antibodies that neutralize these pathogenic effects,” he told Healthline.
His team’s clinical trials have been promising.
“When we continued with the MRI analysis and studies we had made, we saw after one year that there was a clear reduction in thalamus atrophy — known to be the best indicator of the disease progression in MS — but also the same in cortical atrophy and whole brain,” he said.
After two years, 90 percent of participants wanted to continue and were feeling better with the treatment, he said.
“We had strong confirmation that this effect was not transient and by chance,” he said.