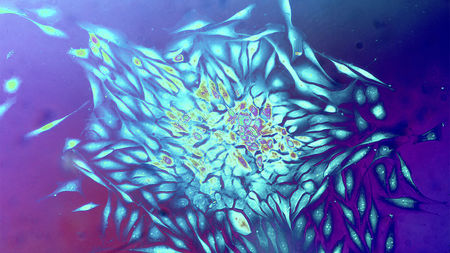
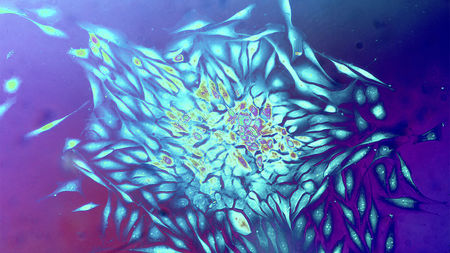
Human breast cancer cells. A huge new trove of data explores how genetic changes drive tumor growth.
Cecil H. Fox/Science Source
The largest ever study to analyze entire tumor genomes has provided the most complete picture yet of how DNA glitches drive tumor cell growth. Researchers say the results, released today in six papers in Nature and 17 in other journals, could pave the way for full genome sequencing of all patients’ tumors. Such sequences could then be used in efforts to match each patient to a molecular treatment.
The Pan-Cancer Analysis of Whole Genomes (PCAWG) project, which had a cast of more than 1300 scientists and clinicians around the world, analyzed 2658 whole genomes for 38 types of cancer, from breast to liver. “What stands out from these studies is the rigor of doing this in a systemic way,” says cancer geneticist Marcin Cieslik, who with colleague Arul Chinnaiyan at the University of Michigan, Ann Arbor, co-authored a commentary on the papers.
Previous published studies—such as those from the U.S.-funded Cancer Genome Atlas (TCGA)—originally looked only at the “exome,” protein-coding DNA that make up just 1% of the genome, of tumors because it was cheaper and easier. But this shortcut left out many changes that might drive cancer growth. With DNA sequencing costs falling, the TCGA and the International Cancer Genome Consortium turned to the entire genome about 10 years ago, sequencing all 3 billion DNA base pairs, including regulatory regions within noncoding DNA, for many tumor samples. These groups also looked for large rearrangements and other structural changes that exome sequencing misses.
The PCAWG study’s 1300-strong team then dug into the data, which the other groups had made freely available in databases. Its analysis didn’t find many new so-called “driver” mutations within genes or noncoding DNA that power cell growth in tumors. But the researchers found “many more ways … to change those pathways” of cancer growth, said project member Lincoln Stein of the Ontario Institute for Cancer Research during a press call. For example, about one-fifth of the tumors had cells in which chromosomes shattered and rearranged, a bizarre phenomenon known as chromothripsis.
Each tumor had four to five driver mutations on average. In all, the PCAWG project was able to find at least one driver mutation in about 95% of the tumor samples, compared with just 67% with exome sequencing, says Peter Campbell of the Wellcome Sanger Institute, another project member. This means many more cancer patients can in principle now be matched to a drug that targets the protein made by that driver gene.
One PCAWG team also figured out how to trace the evolution of the mutations in a single tumor biopsy. The group confirmed that the initial mutations often cropped up years or decades before the cancers were diagnosed, suggesting many could be detected and treated much earlier. Another team found new patterns of mutations that result from environmental exposures such as tobacco smoke. The papers in other journals explore topics such as how often tumor genomes contain DNA from viruses that may have triggered the cancer (13% of the samples).
Some countries, such as the United Kingdom, are moving toward whole-genome sequencing of every cancer patient’s tumor to guide treatment; the full cost is still thousands of dollars per genome, Campbell says. The PCAWG analysis could be “a blueprint for these national programs,” he says. The PCAWG consortium has also begun to pool clinical records and genomes for 100,000 patients to create a “knowledge bank” that doctors could consult to determine the best treatment based on a patient’s tumor genome.
Cieslik and Chinnaiyan note that most of the same information could be gleaned by combining exome data with cheaper tests such as RNA sequencing and assays for rearrangements. “Whether whole-genome sequencing is ultimately the best method in the clinic remains to be seen,” Cieslik says. But the wealth of data from the PCAWG study, which is now freely available to researchers, will help biologists understand the mechanisms of cancer, they say.
Another caveat is that although targeted drugs can be less toxic and more powerful than chemotherapy, most patients’ tumors grow back as a few cells that resist the drug begin to expand. The patient may then need another drug to kill the resistant cells. “It’s certainly true that this kind of sequencing will not mean that all cancers are cured,” Campbell says. “But it points us to where we should be thinking about developing drugs for preventing resistance or treating it once it arises.”