The nation’s ambitious precision medicine program—the All of Us Research Program—is on target to enroll at least 1 million people in the United States who will help accelerate biomedical research and improve health.
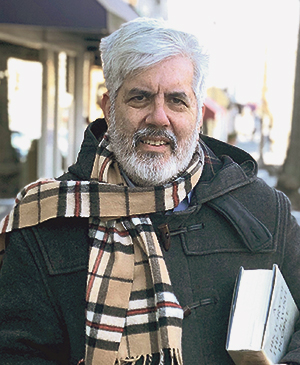
In this week’s New England Journal of Medicine, All of Us investigators, including David Goldstein, PhD, director of the Institute for Genomic Medicine at Columbia University Vagelos College of Physicians and Surgeons, report that more than 170,000 participants have enrolled in the program and submitted health data and DNA. More than 80% of these participants belong to groups that have typically been underrepresented in medical research.
A large portion of the program’s participants and its diversity is provided by New Yorkers who sign up for the program through the All of Us NYC Consortium, led by Goldstein and his fellow principal investigators Ali Gharavi, MD; George Hripcsak, MD, MS; Rainu Kaushal, MD, MPH; M. Elizabeth Ross, MD, PhD; Rhonda Trousdale, MD; and Louise Bier, MS. (The NYC Consortium is centered at Columbia University Irving Medical Center, Weill Cornell Medicine, NYC Health + Hospitals/Harlem and NewYork-Presbyterian).
More than 17,500 New York City area residents have enrolled and over 85% of participants are from communities that have been underrepresented in biomedical research, representing diversity in race/ethnicity, age, sexual and gender minorities, and socioeconomic status.
Longitudinal studies that follow people over time—like the famous Framingham Heart Study that started in 1948—have dramatically improved the prevention and treatment of diseases. But most of these studies have almost exclusively focused on individuals of European ancestry.
“Some findings from these studies are not as applicable to other groups,” Goldstein says. “The All of Us Research Program is an amazing opportunity to bring together the communities we serve and our research community to advance health.”
Goldstein spoke with the CUIMC Newsroom about the progress being made by All of Us, how it will benefit New Yorkers, and what local researchers have to gain from Columbia’s participation in the country’s signature biomedical research effort.
There are several All of Us consortiums around the country that are enrolling participants into the program. Is there anything unique about the New York consortium?

One of the important contributions of the New York group is that the participants we enroll are among the most diverse enrolled at any of the sites in all sorts of ways, including socioeconomic status and geographic ancestry.
It’s important that the participants we enroll come from the communities that we serve so that all New Yorkers can benefit from the research advances in All of Us. That means that we’ll be bringing precision medicine into these communities.
And because we’re enrolling patients from a tertiary care center (NewYork-Presbyterian), we’re also increasing the diversity of the kinds of medical conditions that we can study with data from All of Us. There are some other really big genetic studies going on now—like those led by Regeneron and Geisinger and the UK Biobank—but these do not draw from patients who are seen at tertiary care centers. So that diversity, I think, has been underrepresented in large scale genomic datasets so far.
How can Columbia clinicians and researchers make the best use of the data being collected from their patients?
We’re building a resource that really should empower local research for years or decades to come. It’s important that our community of clinicians and researchers understands what the program is, what data will be generated on our participants over time, and what our ongoing relationship with our participants is going to be so they can tap into the resource to answer their own research questions that will lead to new insights into human biology and improved patient care.
We have a very large number of participants—tens of thousands of our patients—who are providing a lot of information about their genetics, lifestyles, and medical histories. Some even have wearable devices collecting information. They all have a willingness to respond to follow-up questions or come in for follow-up evaluations that might be triggered by genomic or other findings. And I think the real benefit—to our community—will come from our own researchers figuring out really creative ways to make use of the resource.
The program involves a lot of preparatory work and then things will start moving quickly. It’s a little hard to know when we’ll make that transition from prep work to the generation of more valuable data, but I think genomic data will hopefully start to be generated relatively soon.
One of the goals of All of Us is to share any findings that may impact health with participants. Is that expected soon? And what are the challenges of providing genetic data?
Exactly what data to share and how to share it is still being worked out, but there is certainly broad expectation that some genomic data will be shared before too long.
And that also represents an important contribution by the program to precision medicine, because we will see increasing numbers of people who have access to their genetic information. And we have to figure out how to help them make effective use of the data.
This is challenging on a scale as large as that of All of Us, and genetic data can often be complex and have implications for not just a participant, but their family members. The All of Us Research Program is working to ensure that participants have access to genetic counseling services so they can put any findings into context for themselves and their families.
Precision medicine—and All of Us—have been criticized for expecting too much from genetic data. Why do you think they’re wrong?
There are a lot of different criticisms of precision medicine, but maybe the most reasonable one is how helpful precision medicine approaches will actually end up being.
Right now, the domain of the application of precision medicine is very narrow. The classic example is: there’s a child, they’re really sick, you don’t know why. You look at their genome, you find a cause, and you hope that points you to a therapy. That of course happens, but this archetypical example represents a very small proportion of people that are sick.
I think that there are signs that we just don’t know enough yet to apply precision medicine as broadly as it could be. In our own work at Columbia, we’ve seen that even in a common condition like chronic kidney disease, the genomes of patients can reveal differences amongst patients who otherwise seem similar to each other, and those genetic differences directly impact their treatment.
This wasn’t a rare, childhood genetic disease for which precision medicine has been shown to work; this is a common, often adult-onset condition. So, I think precision medicine will be more broadly applicable than some critics have argued.
To figure out which diseases precision medicine approaches can actually help, we really have to better understand how patients differ from one another. And in order to do that we need very large datasets with a lot of “omic” information that can help us differentiate patients. And we need a lot of information about what those patients are like, how their disease presents, how they live their lives, so that we can uncover how disease is influenced by interactions between genetic risk factors and the environment. And, of course, we want this kind of information not only for patients after they present with disease, but for people before they present so that we can develop precision medicine approaches to disease prevention.
At this stage, we can’t prove that precision medicine will be useful for a broader array of diseases, but the data that All of Us will be collecting are what we need to find out.
So far, we’ve talked about precision medicine as something that’s applied after a person has developed a disease. What about predicting disease?
In a broad range of clinical areas where there are genomic studies going on now, we can see that we can meaningfully distinguish patients genetically. When we look at patients with chronic kidney disease, for example, we see lots and lots of different genetic causes of disease.
But it’s clear that we’re not as good at the genetics as we need to be. When we look at people who don’t have chronic kidney disease, we also see lots of causes of kidney disease! Not as many, but a lot. And we don’t know what to make of it, or what to do about it.
So, what I hope that we deliver with All of Us is a dramatic improvement not only in our ability to use genetic information to better treat disease, but also, critically, to prevent disease. And this is really an essential point to emphasize.
We’re not very good right now at taking a person who is healthy, looking at their genomic information, and working out that they have a high risk of certain diseases and then preventing that disease.
That’s a harder thing to do with the genetics, and it’s my hope that All of Us will make such an important contribution in how we do genetic studies that we not only get better at diagnosing causes of disease and stratifying disease populations, but we get good enough at the genetics to really move meaningfully into disease prevention that is genomically informed.