A research team at in Belgium has recently created a DNA injection that can induce the production of new antibodies, marking a milestone in the development of antibody gene therapies. This technique is much more affordable and scalable than the current laboratory approaches to synthesizing antibodies for pharmaceutical use. This treatment was found to be effective in a preclinical trial involving sheep, the findings of which were published on September 10 in .
What is the Antibody Gene Therapy?
The antibody functions within our immune systems to defend against bacteria, viruses, and other pathogens. These proteins are created naturally by the human body but have are also developed industrially to create immune therapies for cancer and various infectious diseases. Synthesizing these antibody drugs requires massive bioreactors that house thousands of gallons in volume, making this process expensive and complex. As a result, these biologic treatments can often cost users thousands each month. Being that the instructions for antibody synthesis are encoded within genes, an injection containing the DNA code for an antibody could potentially be given to a patient to make them naturally produce this protein.
Led by Professor Kevin Hollevoet and Professor Paul Declerck of the Laboratory for Therapeutic and Diagnostic Antibodies at KU Leuven, and with collaboration provided by Dr. Nick Geukens of PharmAbs, a research team has recently created an injection that can induce this antibody synthesis within one’s body. Moving this antibody generation from the laboratory setting to the patient’s body has the potential to significantly cut the cost of these antibody treatments. The benefits of this DNA injection also outlast those of the industrially produced antibody injections, leading to fewer required treatments in patients and increased access to biologic medications.
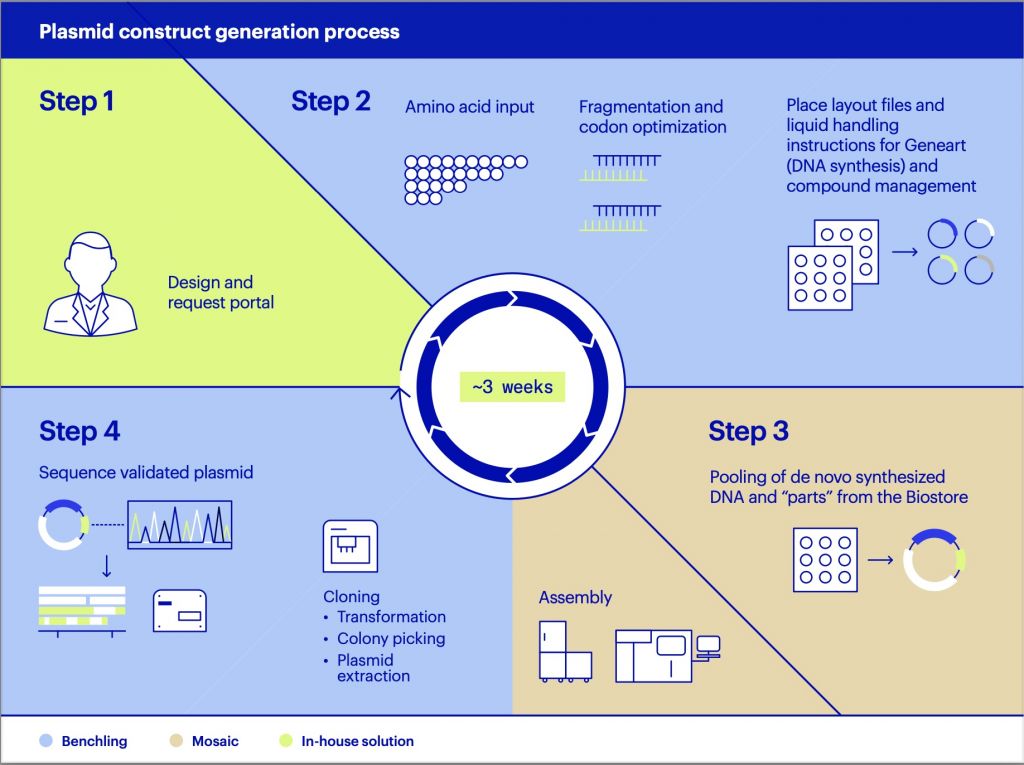
“Just like other proteins, each antibody has a unique DNA code with building blocks and instructions,” explained Hollevoet. “To get this information into the body, we put the desired code in a specially developed plasmid, which is a circular string of DNA. The plasmid functions as a vehicle for the DNA code.”
Administering the DNA Injection
The antibody gene therapy is given through an intramuscular injection, followed by electrical stimulation that produces little to no pain. The purpose of this latter step, known as electroporation, is to increase the muscle cells’ permeability to the injected genetic components. Once within the cells, this DNA is transcribed into mRNA in the nucleus, which is then translated by ribosomes to form antibodies in the cytoplasm. Finally, these antibodies enter the bloodstream, where they can begin to combat disease.
“There have been several successful studies in the past on mice, including by our research group,” said Hollevoet. “But we didn’t know whether this approach would work on humans, since they are much larger in size.”
To address this clinical discrepancy, the KU Leuven team evaluated the technique in sheep, being that this animal models the human distribution of weight, blood volume and muscle mass. After receiving the DNA injection, the sheep displayed antibody concentrations in their blood that was deemed therapeutic. These antibodies were detected in the animals for nearly one year after the initial injection as well. The researchers noted that these animal models could also be used to test potential DNA medications, lowering risks imposed upon clinical trial participants.
“The fact that this technique also works in larger animals shows that this kind of treatment could be possible for humans. It’s a milestone for antibody gene therapy,” explained Declerck.
Going Forward with the Treatment
Currently, the team is collaborating with several research groups and companies to expand upon their antibody gene therapy. They note that selecting the best-fit antibody is one of the more significant challenges in their work.
“In principle, we can inject the DNA code of any antibody, but we focus on diseases where this approach can help patients the best,” claimed Hollevoet. “Currently, we are mostly focused on cancer treatments, among others immune therapy. We also see possibilities for infectious diseases like HIV and the flu, and neurological diseases like Alzheimer’s. Even though there are still roadblocks on the way to using this treatment in humans, the finish line has never been so close.”