A U.S. military research program that seeks a new way to boost a body’s immunity to viruses could change how governments and militaries prepare for pandemics — and might even arrive soon enough to help with the COVID-19 outbreak.
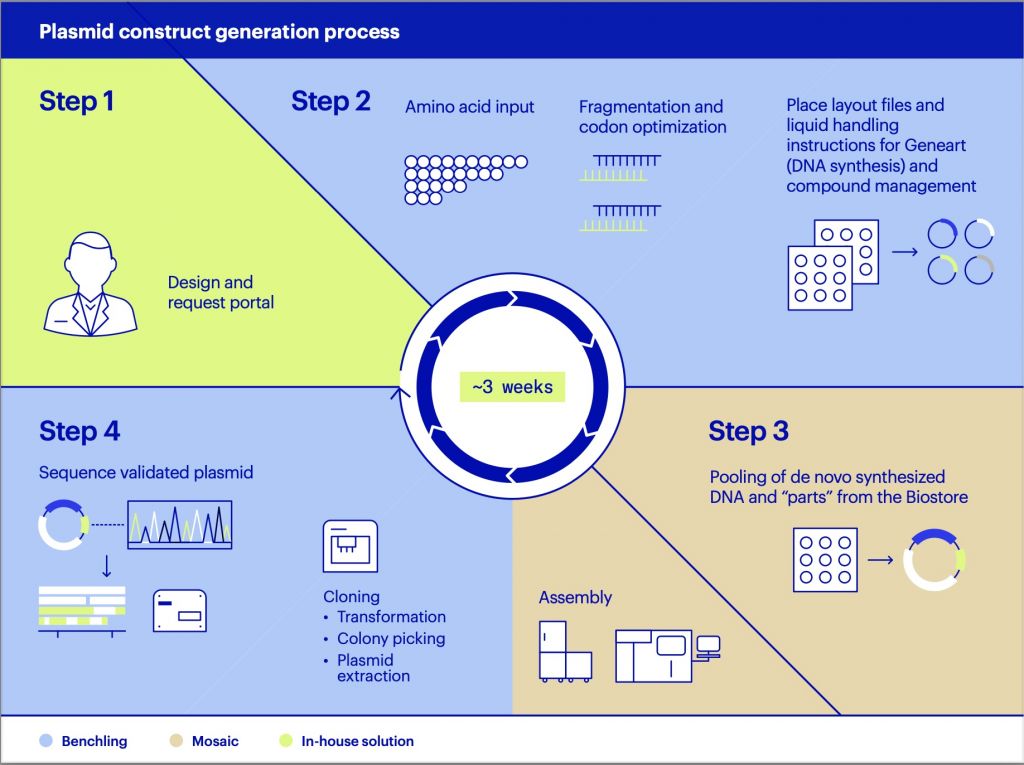
DARPA’s Pandemic Prevention Platform isn’t looking to create a vaccine, which can take years to produce and weeks to take effect in the body. Rather, the goal is to identify the specific monoclonal antibodies that the body naturally produces when it encounters a virus, and then trick the body into producing the one that guards against a specific illness. That could serve as a temporary, months-long shield that can protect the individual from the pathogen until a vaccine can be brought online.
But these antibodies “take a long time to find and discover. There’s a long pipeline in the biomedical world to identify and test them and really understand these antibodies,” said Dr. Amy Jenkins, who manages the program at DARPA.
One of the goals of the program is to accelerate the discovery process.
“We have really trimmed that timeline down from what is usually multiyear timeline to just being a several week timeline,” Jenkins said on Monday.
It’s a feat they’ve achieved through investments in microfluidics, the manipulation of liquids at the sub-millimeter range; nanofabrication, the fabrication of objects less than a billionth of a meter in size; and new approaches to gene sequencing.
Jenkins described it this way: “We are able to take a patient that has recovered from this pathogen, for example, and we are able to sequence many of of their B cells. So those cells that make those antibodies that help protect you against those pathogens? We are now able to sequence all of those because of next-generation sequencing approaches.”
But they have very little of the B-cell sample to work from: just one sample from a single individual. If that person’s antibody response was relatively weak, there will be less antibody material to find. “We are relying on that one patient’s immune response. We would typically do this for anywhere between five and ten patients. We have one. So if that one person had a really robust immune response, that’s going to be great. If they didn’t because some people just respond differently, we could be in trouble, because it may be hard to find an antibody. Preliminary data suggests that there may be antibodies present. We are optimistic but also cautious that the antibodies are there,” she said.
The second goal is to accelerate the delivery of manufactured antibodies. Like vaccines, antibodies are produced in bioreactors, basically a giant, complex cell culture that plays the role of the human body.
Jenkins and her collaborators are trying to invent a new way to produce antibodies at scale by using the RNA and DNA code of those COVID-19. When that RDA or DNA is injected into a patient, it would begin to work immediately, helping health people ward off the virus and perhaps even functioning to treat sick people as well.
It’s the difference between buying a piece of furniture already assembled versus a mail-order kit with an instruction manual. The hope is that the body will be able to construct the response itself. In essence, said Jenkins, the body becomes the bioreactor. Since RNA and DNA is much easier to produce than a traditional vaccine, the hope is to drastically cut down on the time to manufacture.
Related: Defense Firms Limit Travel, Adapt As Coronavirus Spreads
Related: DOD, Feds Issue Coronavirus Guidelines for Civilian Employees
Related: The US Has Tested Fewer than 5,000 People for the Coronavirus — and That’s a Big Problem
“Right now, we aren’t there. The manufacturing timeline has shrunk but we think it would take us a minimum of 90 days to manufacture an RNA today,” she said.
The more immediate goal for the COVID-19 outbreak is to discover the antibodies that are relevant to the illness and then produce those in a traditional bioreactor, hopefully quickly. They could then go to frontline medical workers, deployed troops, or even to sick patients to treat the infection. The hope is “to have something by late summer” she said, but that’s if everything goes perfectly.
Inside the Pentagon, officials are also taking precautions. Defense Secretary Mark Esper has implemented the CDC’s “social distancing” guidelines, which suggests people stand six feet apart from one another. This week, Esper held his Monday-morning meeting with senior officials including Chairman of the Joint Chiefs, Gen. Mark Milley, occurred via video conference as part of the new procedures.
“We’re encouraging everybody to practice good social distancing, using their judgment and within the bounds of what we can do to continue to do the job,” said Pentagon spokesman Jonathan Hoffman.
Katie Bo Williams contributed to this report.